Delirium – Antipsychotic Flowchart and Pharmacologic Management
Key concepts in prescribing antipsychotics for delirium:
- No antipsychotic is thought to be superior
- Selection should be based on indication, comorbidities, and side effect profile. For example, a patient with orthostatic hypotension or urinary retention should avoid quetiapine and olanzapine given the anticholinergic and orthostatic effects while a patient with a borderline prolonged QTc should avoid ziprasidone.
- All antipsychotics are off label in the treatment of delirium
PEARL: Antipsychotics may prolong delirium and have a black box warning due to increased mortality of ~1.7x (2.6 –> 4.5% over 10 weeks) in older adults with dementia.
Consider the use of low dose trazodone as an antipsychotic sparing agent (click to expand)
Trazodone may cause a desired sedation effect with lower comparative risk of harm as compared with antipsychotic therapy.
However, trazodone has not been as rigorously studied in delirium as antipsychotics. Here are some articles:
- Retrospective review: First- and second-line pharmacological treatment for delirium in general hospital setting-Retrospective analysis
- A retrospective review of patients hospitalized in delirium in China found trazodone was used often as a first line agent (51%, n = 100) followed by quetiapine (29%, n = 57). Those treated with trazodone were switched 41% of the time while quetiapine was switched 9%. The duration of use did not vary.
- Prospective secondary analysis of observation study: Low-Dose Trazodone for Delirium in Patients with Cancer Who Received Specialist Palliative Care: A Multicenter Prospective Study
- A secondary analysis of a prospective observational study found that in 38 patients treated palliative care settings found that delirium severity, sleep-wake disturbance, affect lability, and moto agitation were improved with the main adverse event being somnolence (24%).
- Ongoing ICU RCT at the University of Southern California (TRAQ trial) expected 2023: Trazodone vs Quetiapine vs Placebo for Treating ICU Delirium
We recommend the use of trazodone as an antipsychotic sparing agent.
Other pharmacologic agents commonly considered in delirium.
Trazodone (Desyrel)
Trazodone may cause a desired sedation effect with lower comparative risk of harm as compared with antipsychotic therapy.
However, trazodone has not been as rigorously studied in delirium as antipsychotics. Here are some articles:
- Retrospective review: First- and second-line pharmacological treatment for delirium in general hospital setting-Retrospective analysis
- A retrospective review of patients hospitalized in delirium in China found trazodone was used often as a first line agent (51%, n = 100) followed by quetiapine (29%, n = 57). Those treated with trazodone were switched 41% of the time while quetiapine was switched 9%. The duration of use did not vary.
- Prospective secondary analysis of observation study: Low-Dose Trazodone for Delirium in Patients with Cancer Who Received Specialist Palliative Care: A Multicenter Prospective Study
- A secondary analysis of a prospective observational study found that in 38 patients treated palliative care settings found that delirium severity, sleep-wake disturbance, affect lability, and moto agitation were improved with the main adverse event being somnolence (24%).
- Ongoing ICU RCT at the University of Southern California (TRAQ trial) expected 2023: Trazodone vs Quetiapine vs Placebo for Treating ICU Delirium
We recommend the use of trazodone as an antipsychotic sparing agent.
Valproic acid (Depakote)
Valproic acid has been used as an adjunct in delirium or in those who cannot tolerate antipsychotics (such as in the case of prolonged QTc).
There is potentially promising data behind the use of valproic acid in delirium. However the data is sparse, observational (case series and retrospective cohort), and potentially confounded by organ failure, polypharmacy (high dose benzos and substance use). In addition, the metabolism of valproate is through cytochrome P450 which can result in altered metabolism of common medications such as aspirin and ibuprofen.
Here are some selected articles:
- Valproic Acid for Treatment of Hyperactive or Mixed Delirium: Rationale and Literature Review
- Delirium in the Intensive Care Setting: A Retrospective Analysis
- Prescribing Practices of Valproic Acid for Agitation and Delirium in the Intensive Care Unit
- Effectiveness of valproate on delirium and/or aggressive behavior in demented patients: A practical pilot study
- Delirium – The American Journal of Psychiatry (Under ‘Antiepileptics’)
We recommend against the use of valproic acid.
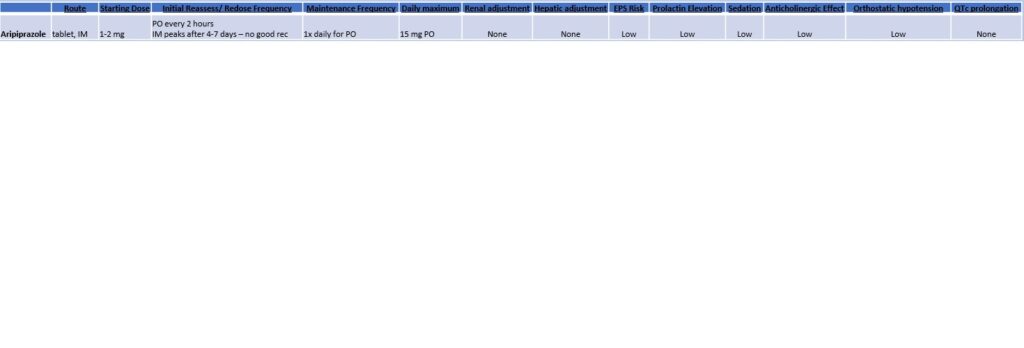
Aripiprazole (Abilify)
- Aripiprazole is a hypothetically attractive antipsychotic choice because it may have the lowest risk of QTc prolongation and has a more favorable side effect profile.
- However, it has not been as rigorously studied as other antipsychotics in delirium and its use is complicated by a long half life. The long half life creates difficulty in potentially reaching a steady state, redosing the medication, and there is no clear guidance on non-oral formulations which may be needed in a patient unable to take oral.
In our experience, it may be reasonable to use aripiprazole as it tends to be well tolerated but is of questionable efficacy
Melatonin and other melatonin receptor agonists
Melatonin is a hormone produced in the pineal gland that helps with circadian rhythm and sleep.
Prevention of delirium
There is some (mixed) data that suggests melatonin might prevent delirium
- Exogenous Melatonin for Delirium Prevention: A Meta-analysis of Randomized Controlled Trials – 2015. This meta-analysis found 4 RCTs with 669 older adults that showed a trend towards reduced delirium (RR 0.44, CI 0.15-1.13, p = 0.08). The reduction in delirium was seen in medical patients (RR 0.25, CI 0.07-0.88, p = 0.03) but not surgical.
- Melatonin and sleep in Preventing Hospitalized Delirium: A Randomized Clinical Trial – 2018. In a small study of 69 patients admitted to the medical unit, a dose of 3 mg did not significantly prevent delirium or improve sleep.
- Melatonin for delirium prevention in hospitalized patients: A systematic review and meta-analysis – 2021. This metanalysis found 14 RCTs with 1712 participants. Melatonin or ramelteon reduced delirium in surgical (49%) and ICU (34%) patients (RR 0.61, CI 0.42-0.89, p = 0.009) but not medical patients.
- The effect of melatonin on delirium in hospitalised patients: A systematic review and meta-analyses with trial sequential analysis – 2020. After reviewing 16 RCTs with 1634 patients, the authors found results that neither support nor oppose the use of melatonin due to high heterogeneity and low certainty.
- The Prophylactic Melatonin for Delirium in Intensive Care (ProMEDIC) is a multicenter randomized double-blinded, placebo trial will hopefully give a more definitive answer in ICU patients.
Treatment of delirium
Delirium – American Journal of Psychiatry (Section on Melatonin) – 2019. Authors concluded that “little is known about the efficacy of melatonin for the treatment of delirium once it has developed” and that further research is indicated due to the favorable safety profile.
We recommend using melatonin given the potential benefit (though there is mixed data) to prevent and treat delirium balanced against the excellent safety profile.
Dexmedetomidine (Precedex) and other alpha2-adrenergic agonists
Dexmedetomidine is a selective alpha2-adrenergic receptor antagonist that has both analgesic and sedative properties. As such, it may spare the use of potentially deliriogenic medications such as opioids and benzodiazepines. The use of dexmedetomidine is limited by bradycardia, hypotension, cost, and need for ICU monitoring. Clonidine has less CNS selectivity but is oral and may be used in non-ICU settings.
Prevention of delirium
- Two studies comparing dexmedetomidine with benzos, lorazepam (JAMA 2007) and midazolam (JAMA 2009), showed lower rates of delirium.
Treatment of delirium
- Effect of dexmedetomidine added to standard care on ventilator-free time in patients with agitated delirium: a randomized clinical trial – 2016. 74 patients ready with delirium and agitation who were otherwise ready for extubation were randomized to placebo or dexmedetomidine. Those receiving dexmedetomidine were more likely to have more ventilator free hours (17 hours, CI 4-33.2, p = .01)
We recommend dexmedetomidine as an alternative in the ICU to achieving sedation through other potentially deliriogenic medication such as benzodiazepines. It is unclear how it compares to antipsychotics.
Thiamine
The role of thiamine is well summarized in Delirium – The American Journal of Psychiatry (2019) under “Thiamine”:
“Nutritional deficiencies, particularly of the B vitamins, have been associated with delirium. Thiamine (vitamin B1) deficiency can lead to a spectrum of mental status changes, including Wernicke’s encephalopathy (triad of nystagmus, ophthalmoplegia, and mental status changes), Korsakoff’s syndrome (irreversible memory impairment, usually as a consequence of untreated Wernicke’s encephalopathy), and delirium. Although the most common cause of thiamine deficiency is alcoholism, a variety of conditions that result in malnutrition, including conditions that result in poor feeding, such as anorexia nervosa and orofacial cancers; conditions that limit absorption, such as gastric bypass surgery, gastric cancer, and colon cancer; and hyperemesis gravidarum, can cause thiamine deficiency… If thiamine deficiency is suspected, patients should be treated with 250 mg/day of thiamine intravenously for 3 to 5 days.“
There is some early, limited evidence that thiamine in select populations may reduce post-operative delirium (Thiamine for Prevention of Postoperative Delirium in Patients undergoing Gastrointestinal Surgery: A Randomized Clinical Trial – 2020) or in critical illness (Delirium in Critical Illness Patients and the Potential Role of Thiamine Therapy in Prevention and Treatment: Findings of a Scoping Review with Implications for Evidence-Based Practice). However, we are not aware of large, high quality RCTs to support or oppose the use of thiamine to prevent or treat delirium.
We recommend thiamine supplementation in clinical scenarios concerning for thiamine deficiency.